Surviving and Healing: A Therapist’s Second Battle with Hyperemesis Gravidarum

This is a story of survival, resilience, and healing after Hyperemesis Gravidarum.
Trigger Warning: Pregnancy, medical neglect, medical trauma, mental health struggles (including suicidal thoughts), vivid descriptions of illness, descriptions of nausea, parenting challenges, PTSD, and abortion statistics.

Pictured: One of the many visits from in home nursing to change my IV placement.
Sharing my personal story isn’t something I’ve ever been good at. As a therapist, I’m used to holding space for others, not the other way around. But as a perinatal therapist and two-time survivor of Hyperemesis Gravidarum (HG), I feel a pull to share the raw, messy truth - because HG left me with scars that still ache. And if there’s one thing I’ve learned, it’s that pain doesn’t heal in silence.
Pregnancy is a deeply personal journey, and people struggle in different ways. Some struggle to get pregnant, others to stay pregnant, and for some, the fight is simply to survive pregnancy.
I am one of those who struggles to survive.

Pictured: Another day, another trip to the hospital.
Pregnancy: The Glow I Never Got.
Pregnancy is so often wrapped up in dreamy, glowing images. People gush about the cravings, the kicks, the magical bond. But for some of us, pregnancy is a war zone. For me, it was HG: an unrelenting thief that robbed me of food, comfort, joy, and even hope.
HG isn’t morning sickness. It’s not something that crackers or ginger tea can magically fix. It’s a monster. It’s being so sick you can’t hold down water while everyone around you insists you’re glowing.
It’s vomiting so much your body feels like it’s collapsing in on itself. It’s questioning how much longer you can survive—and if it’s worth it to try.
This wasn’t my first HG battle. I’d been here before, during my first pregnancy. I swore it would never happen again. After five years of healing, therapy, changing providers, and trying to feel like myself again, I decided I was ready to risk it. But HG doesn’t care about your preparation.
Fighting HG - Again.
I knew the stats: Hyperemesis Gravidarum recurs in up to 70% of pregnancies. I prayed I’d fall into the lucky 30% who escape its return, but I knew in my gut I wouldn't be. I prepared for the worst, and I was right to. From days before my missed period until the day I delivered, HG was back, louder and crueler than before.
I lost over 50 pounds—not from dieting, but because my body rejected food with a tragic efficiency. Vomiting became my daily reality. Not once or twice a day, but once or twice an hour, sometimes more. There were only two days in my entire pregnancy that I didn’t vomit multiple times.
I was going to the hospital so often for fluids that I couldn’t bear it anymore. Even though my medical records showed significant weight loss, and my labs revealed clear signs of starvation and severe dehydration, I felt dismissed. I didn’t look like skin and bones, so my condition was often minimized. Sitting in the ER for hours, repeating the same story to skeptical staff, became too much. Eventually, I advocated for home nursing. It was a relief but also a stark reminder of how desperate my situation had become. From there, my living room became my small hospital, with my coffee table covered in infusion supplies. Syringes, IV catheters, gloves, bags of fluids, and Zofran…so much Zofran.
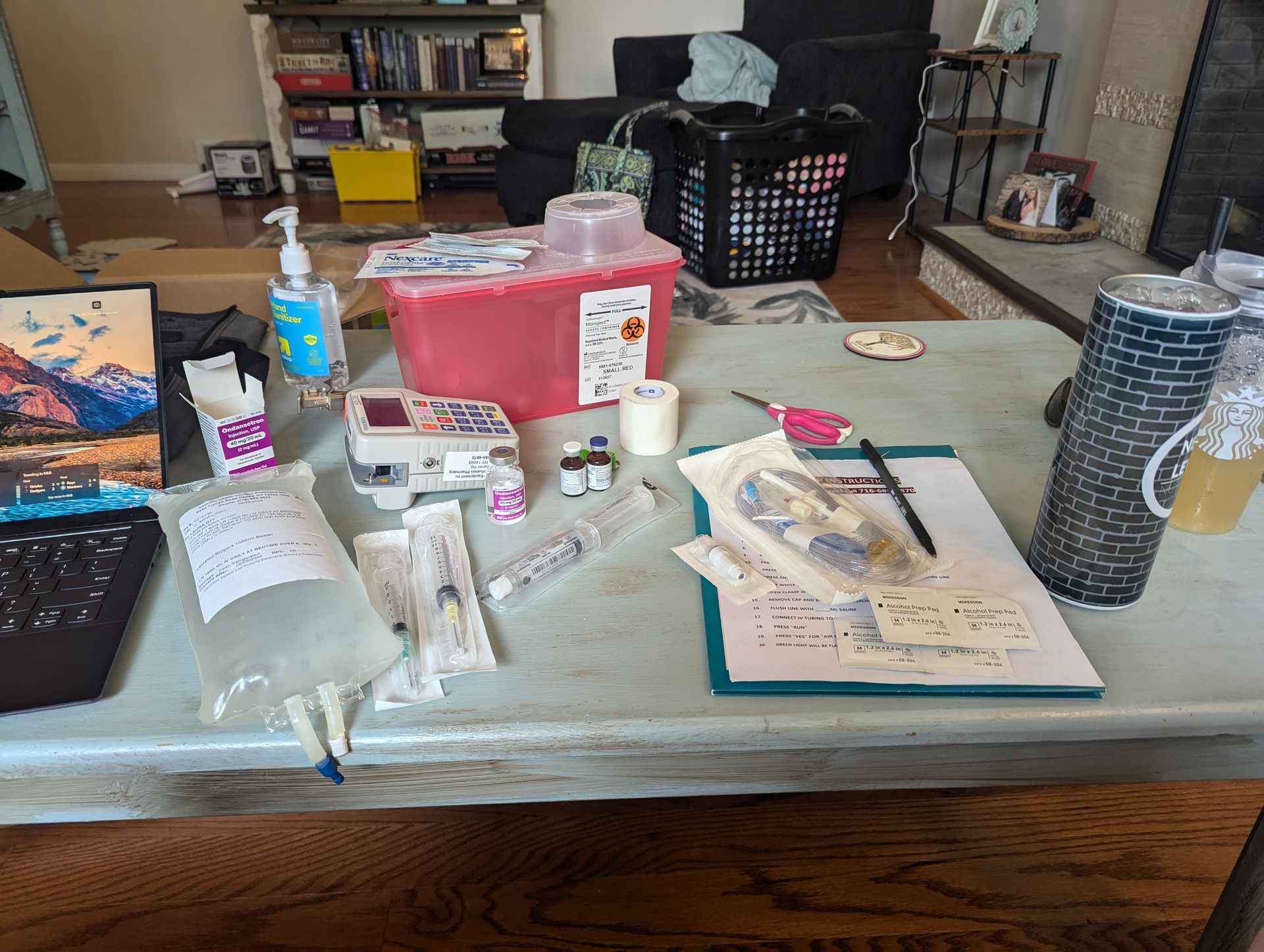
Pictured: My in-home hospital setup.
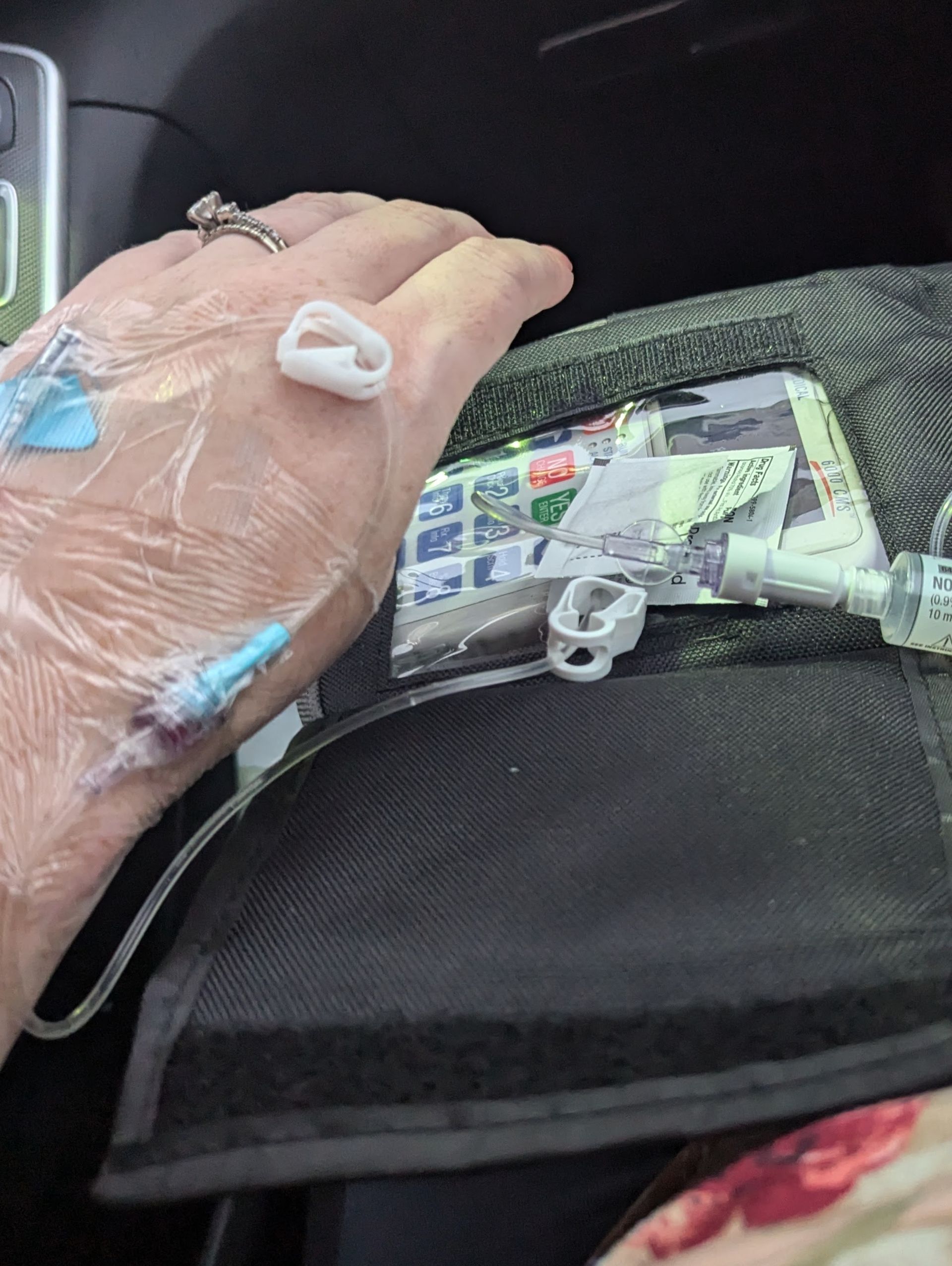
Pictured: Often clearing and capping my IV lines on the go.
The PICC Line: "Can This Wait Until Business Hours?"
After weeks of daily or near-daily IV catheter placements, I ran out of usable veins.
My arms and hands were constantly covered in bruises. My IV sites began to reject, and my veins became so inflamed that fluids would infiltrate my tissue as the catheter would slip out of my vein. The pain of fluids pumping into my tissue felt fiery, radiating through my arm. Even worse, the meds weren't getting where they needed to go. I would call the home care on call and they would ask, can this wait until business hours? I felt guilty saying no. The PICC line became a necessity—both a relief and a sobering acknowledgment of the severity of my battle.
The Hardest Moments
I want to tell you about the moments people don’t talk about—the ones I hate to admit. Like sitting on the bathroom floor sobbing, too weak to stand, cramping from vomiting the nothing left in my stomach.
I’d glance at my phone to see the time, knowing I had to pull myself together, get my daughter ready for school, and be present with clients for nine hours.
I carried my infusion pump with me for 12 hours a day. The incessant beeping when the line got pinched or the bag ran out became background noise. The weight of the pump was a constant reminder of my body’s betrayal—a tether to my illness I couldn’t escape.
(Pro tip: Get hospital-grade puke bags. I kept them in my office, car, and home. HG doesn’t wait for convenience.)
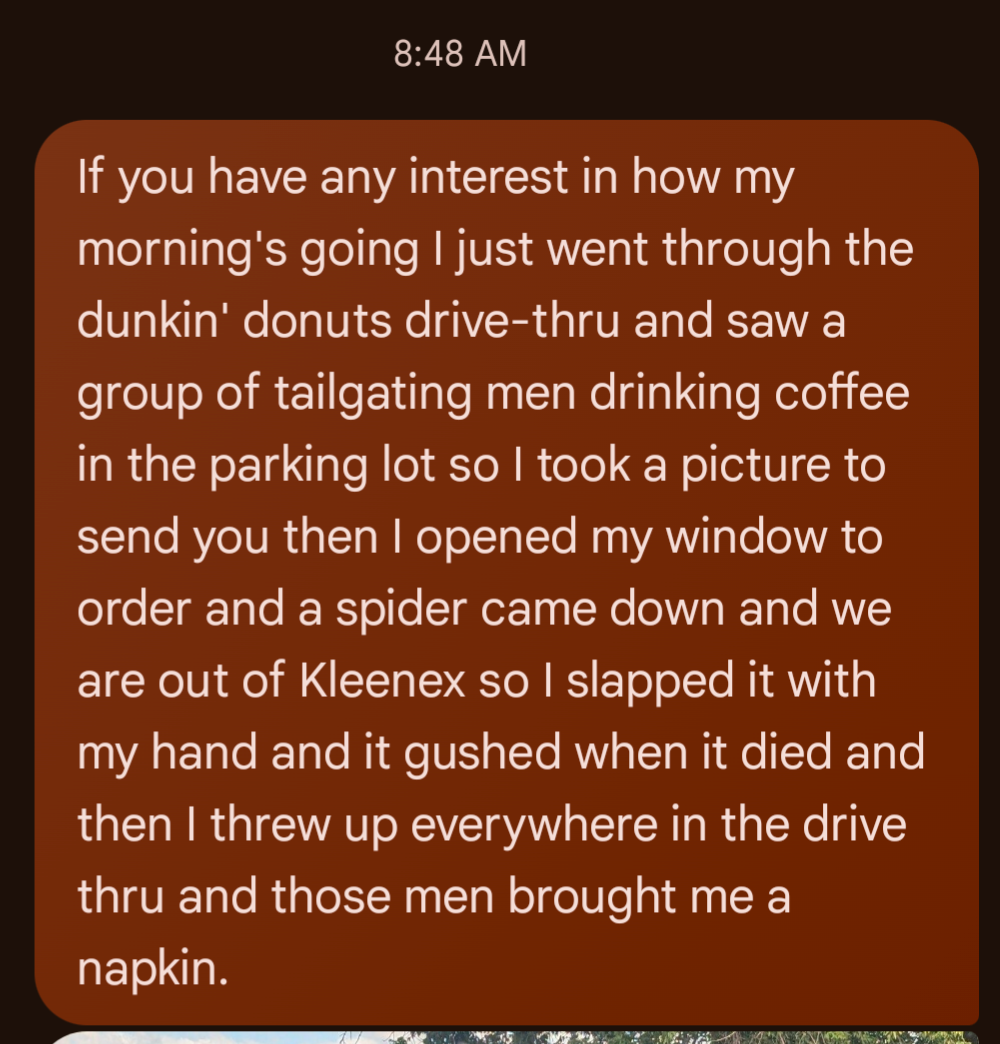
Pictured: Everything made me vomit. Textures, smells, foods... My husband was often the recipient of my texts venting about my most recent struggle.

Pictured: Another ER visit.
The Mental Toll
HG doesn’t just break your body; it takes over your mind. The thoughts I had scared me:
“I deserve this for thinking I was strong enough”
“I’m failing my baby before she even arrives.”
“I am stupid to think I could do this again.”
“The universe doesn’t want me to be a mom. I'm not meant for this.”
HG can feel impossible to endure. Nearly 5% of women terminate wanted pregnancies, and over half consider it. Statistics show that 25.5% of HG sufferers experience suicidal thoughts. I’ve been one of those women. The desperation and hopelessness are suffocating.
As a therapist, I know how powerful it can be for perinatal clients to feel seen. Sharing these struggles isn’t just about me; it’s about giving others permission to be honest about their own battles.
The Things That Kept Me Going
Therapy: My lifeline. A space to cry, rage, and just be. Even if it's just a quick teletherapy call this can be so helpful when you need it the most.
Community: Online HG support groups reminded me I wasn’t alone. The
HER foundation is also chock-full of resources and information on Hyperemesis Gravidarum, so if this is something you are experiencing yourself, or a loved one is experiencing, it is worth checking out.
Small Wins: Finishing half a smoothie before vomiting? A victory.
Self Advocacy: I demanded better care in spaces that minimized my suffering.
Compassion: I reminded myself, “You’re doing your best, and that’s enough.”

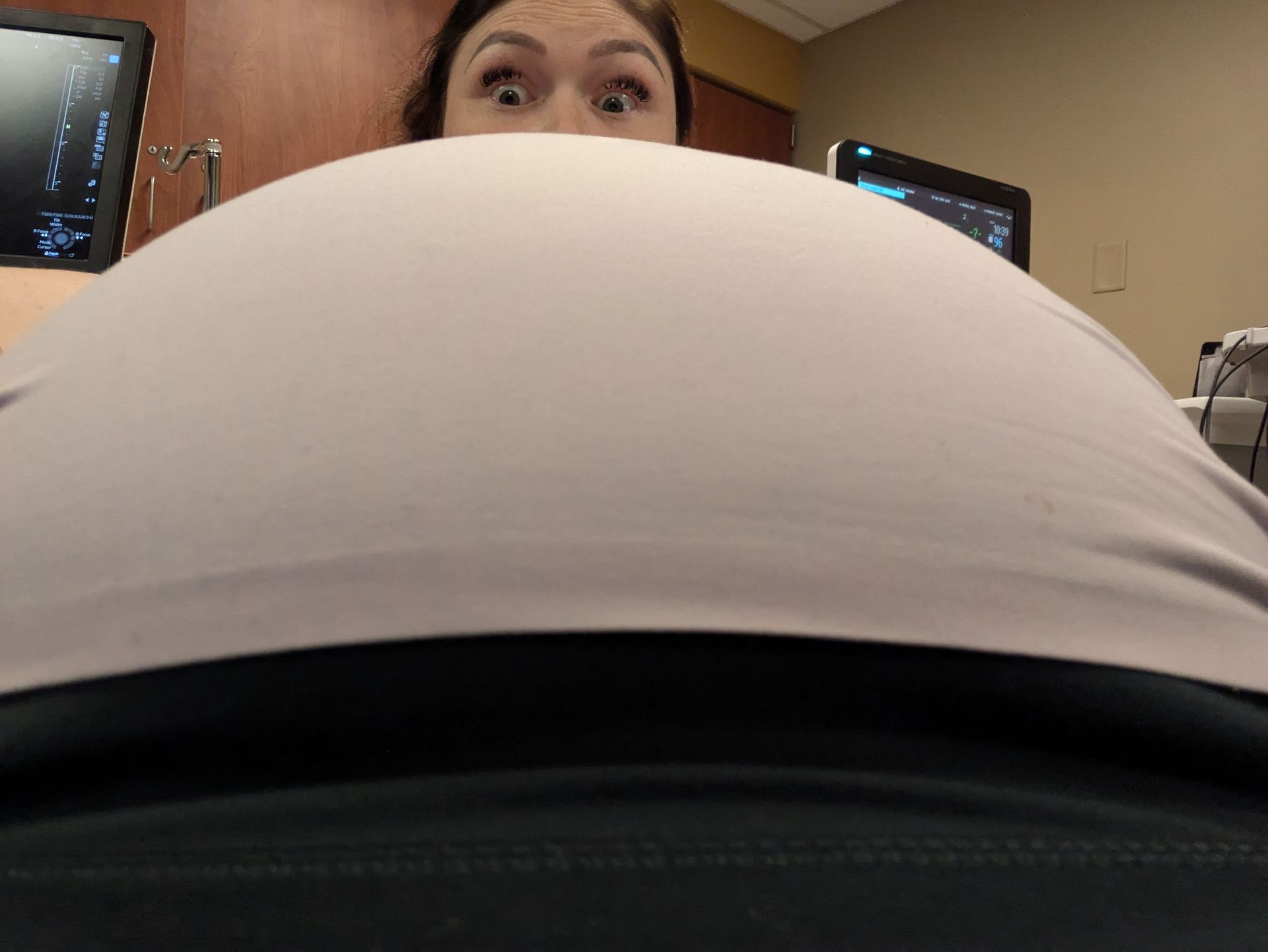
Pictured: When I arrived at the hospital for my induction hoping the end was in sight.

Pictured: Enjoying my girls, whose pregnancies brought me immense suffering but whose existence brings me irreplaceable joy.
Postpartum: Picking Up the Pieces.
Now that I’m postpartum, I’m rebuilding. Society celebrates my smaller body, but I don’t. Pre-pregnancy, I felt strong. Now, I feel weak and exhausted.
I stopped pumping and breastfeeding after six weeks—a decision made out of self-care and necessity. I needed my body to feel like mine again, free from the machines and exhaustion that defined my pregnancy. That choice has helped me reclaim my body, slowly but surely.
The trauma of HG doesn’t disappear after delivery. It lingers, sneaking into quiet moments. But I’m learning to honor what I survived and give myself the space to heal.
To the Ones in the Trenches
If you’re battling HG or simply trying to survive whatever journey you’re on, hear this:
You are not weak.
You are not failing.
You are surviving something unimaginably hard.
This journey isn’t easy, and it doesn’t magically end when your baby arrives. HG takes so much, but it doesn’t take everything. Even when it feels impossible and neverending, there is hope.
As I hold my baby, I see the light I fought for. While I wouldn’t wish HG on anyone, I’m proud of the warrior I’ve become. And my hope is that you know you are worth advocating for.
Nature's Symphony
Those hospital grade puke bags came in clutch on the road.
Faces of Humanity
A site that started infiltrating.
Sands of Time
There's no time off from being a Mom.
Beyond Boundaries
I had to find humor to survive. Pre PICC line belly selfie.
Constant bruises from attempted and failed IV's.
Ott Counseling is a mental health counseling office located in Cheektowaga New York. We have several therapists who specialize in perinatal and postpartum mental health, perhaps out of an abundance of awareness of how pregnancy, birth, and postpartum impact the mental wellbeing of women and their families. We offer both teletherapy and in-person appointments for clients in Western New York and New York State suffering from Hyperemesis Gravidarum, as well as a termination of a desired pregnancy due to complications with HG. We are here to give you a couch to cry on, and are more than happy to lend you a barf bag, or pause our session to help you run to the restroom for the quick in-session vomit whenever necessary! Please Call Us or Contact Us through our website for more information on support options, and make sure you check out the HER Foundation for more Hyperemesis Gravidarum resources and information!